In January this year Professor Christian Marescaux, a neurologist at the main public hospital in Strasbourg in north-east France, accused the institution of allowing private patients to queue jump stroke victims who were in urgent need of MRI scans. Today, six months after first going public on the scandal in an interview with Mediapart (read here in French), he reflects on the character traits that led him to blow the whistle in the first place. “I don't have that way of being cool, supposedly balanced, that allows you to put everything into perspective...you have to have a certain rigidity of character to be unable to bear injustice,” he says.
As head of neurology at the Strasbourg CHU teaching hospital, Professor Marescaux was responsible for the cerebro-vascular accident unit, a position he has since relinquished. Despite his whistleblowing and complaints by three patients, he says, nothing has improved. Indeed, he believes the situation has got worse.
“I don't exist any more. I no longer have any authority over my department. I just do my consultations and university courses,” says Professor Marescaux. “The hospital can say it's my choice because I agreed to take a step back. If I'd continued to run the CVA unit, it would have been a handicap for patients. But it has changed nothing. The difficulties of access to MRI [scans] have increased (...) in-house doctors are refusing the join the department, three jobs are vacant.”
Moreover, the Strasbourg CHU neurology department recently lost its head of neurosurgery, who died at the end of May after a heart attack. His family gave Mediapart permission to report what he had said during an interview in January on condition that his name was not given. He had told Mediapart of his “professional suffering”.
“You constantly have to go and see people, discuss, insist, to obtain an MRI [scan]. For a tumour we're given an appointment in two or three weeks. That's too late!” said the head of neurosurgery. “And we are being refused MRIs for post-operational checks. We've been working like this for years, in a second-class way, yet we are really fighting for our patients. The situation has become even more difficult over the past year, it's unbearable.” In January the neurosurgeon said he was both sorry and pleased that the conflict between Strasbourg CHU’s neurology and radiology departments had been made public. “At least it will change,” he said. But it seems he was wrong.

Enlargement : Illustration 1

Meanwhile, in Saint-Malo, Brittany, in western France, Dr. Jean-Jacques Tanquerel has been fired from his job as head of the ‘medical information department’, the département de l’information médicale, or DIM, at the main public hospital. Tanquerel had tried repeatedly to prevent the contracting out of named patient files to a private company, saying it breached patient confidentiality (1). He finally obtained support from the doctors' professional body, the Ordre des Médecins, and an official recommendation from the national data protection commission the CNIL that the hospital should end the practice. Mediapart reported on Tanquerel's campaign in October 2013, and he, too, says that nothing has improved since then.
“I have been sidelined since January. I have a job as chief medical officer, an office, but nothing to do. I receive no phone calls, no mail, I have no professional relationships,” he says. And the private company whose practices he denounced still works for Saint-Malo Hospital under the authority of a new DIM chief who is more accommodating. The hospital's management tried to get Tanquerel to leave by offering him other jobs, which he turned down “because no justification was given for evicting me from the DIM job, I was not accused of any misconduct.”
Enlargement : Illustration 2
In the meantime the doctor has used his time to write a book, Le Serment d’Hypocrite ('The Hypocritical Oath') in which he outlines the central role played by DIM doctors in the management of a hospital and the pressure they are under at a time of budgetary restrictions. In the system of financing that was introduced into French hospitals in 2007, under which funding is based on the number and nature of medical acts and procedures carried out, hospital budgets depend on the work of DMI doctors encoding these acts and procedures in the computer system .
He also describes a downward spiral that pushes most French hospitals, both public and private, to abandon the most basic ethical rule of patient confidentiality. There is a very fine line, he explains, between optimisation of these payment codes and 'over-coding', which amounts to defrauding the social security system. And he does not hide the threats and intimidation he has suffered, including what he calls being “put to death” professionally.
The hospital sued Dr Tanquerel for libel over his book but lost, and was ordered to pay him 1,500 euros and the same amount to his publisher, Éditions Max Milo. But the regional council of the Ordre des Médecins has now sued him for “untruthful statements and failing in my collegial duty”, he says. “It’s the survival of the fittest. I am discouraged,” he admits.
----------------------------------------------------------
1. The département de l’information médicale (DIM) in a hospital is responsible for the referencing of medical acts and procedures according to a very specific classification of no fewer than 650 description codes set out by the social security administration. These provide the basis upon which it refunds a hospital for the care provided. An increasing number of hospitals engage the back-up services of consultancy companies which offer sophisticated software and expert skills, including those of former healthcare professionals. They are paid between 5% and 6% of the sums they recoup by identifying cases of miss-coding, and have every interest in gaining access to a maximum amount of information about patients’ cases. Private auditing of this kind is perfectly legal as long as the data consulted is of an anonymous nature that describes the medical acts performed per patient, but does not give the patient’s identity. Tanquerel discovered that in his hospital in Saint-Malo the auditors were in fact given access to named patients’ medical files
Young stroke victim's ordeal
No one is suing Professor Marescaux at Strasbourg. Instead he has been the victim of a whispering campaign to discredit him. “The threats are never head on. People are trying to implant the idea of psychological fragility, paranoia. People are saying I was committed to the psychiatric hospital at Rouffach. In reality I worked there for three years, it’s not the same...But the rumours still do the rounds.”
Professor Marescaux took up the case of Alexandra Belhadj, 24, who was diagnosed as having psychological problems when she went to the accident and emergency unit at Strasbourg CHU on April 13th, 2010, although she presented all the signs of a cerebral vascular accident, or stroke. She had an excruciating headache and pins and needles everywhere in her body, and soon became quadriplegic (paralysis of all four limbs or the entire body from the neck down).
She had to wait 16 hours before she was given an MRI scan. But even the scan was wrongly interpreted, and she spent a night alone and unsupervised in a hospital room, entirely paralysed and in respiratory distress. The following day a neurologist finally recognised signs of the stroke on the MRI scan and sent her for reanimation and respiratory assistance. It took many months for her to regain some of her mobility, and she is still 79% handicapped.
The Chambre Régionale de Conciliation et d'Indemnisation CRCI, the body charged with compensating victims of medical errors in France, has taken three years to deal with her complaint, during which time she has been sent from one expert to another for an assessment of her case. The first expert assessment was unfavourable but Professor Marescaux managed to get it overturned. “My father is getting fed up of hearing that his daughter has psychological problems,” says Alexandra Berlhadj. Her father, Noredine Belhadj, himself says: “This hospital treats us like troublemakers. They want to wear us out so we will back down.”
The most recent expert assessment, dating from last April, recognised the delay in providing treatment – previous experts had denied even this. However, it echoed the hospital's lawyer in saying that immediate treatment would not have changed the severity of her symptoms or the gravity of the after-effects she suffered. When this was said during the hearing, a doctor who was not involved in the case commented in front of Alexandra, her lawyer, her family and the entire commission that the affair “stank”.
The CRCI has now finally given its verdict. It has refused any compensation, a decision which Professor Marescaux describes as “staggering”. Alexandra herself is not surprised. “It is incredible and unjust, but so predictable,” she says. “Everyone knows my treatment went from one catastrophe to another, several doctors recognised that. There was no humanity [shown] during my time in accident and emergency. But when you ask the hospital to account for itself, things go from bad to worse. Who could accept that their child would be treated like that by a public service?” She is now considering taking the matter to court, even if she says she no longer has much faith in the system.
At both Strasbourg and Saint-Malo hospitals the consultants have similar explanations for the treatment they have received. Professor Marescaux says that pushing him out and blocking compensation claims by patients is a way of avoiding the underlying problems. For Tanquerel, “the management is trying to make us believe that using this private company, and therefore pushing me aside, is the only way for the hospital to balance its budget. But this is untrue, these companies are very expensive. They should allocate resources to the DIM doctor who should remain the guarantor of patient confidentiality.”
Strasbourg CHU's general manager, Jean-François Lanot, who refused Mediapart's request for an interview, seems unable to resolve the conflict that still plagues the neurology and radiology departments. The regional health management agency, which is responsible for the hospital, appears to be suffering from the same paralysis. Its director, Laurent Habert, also declined to answer Mediapart's questions. At Saint-Malo, Dr Tanquerel notes that the hospital director, Jean Schmid, said of him in front of the whole medical community: “It's him or me.”
'Doctors who question hospitals and the medical profession are intimidated and silenced'
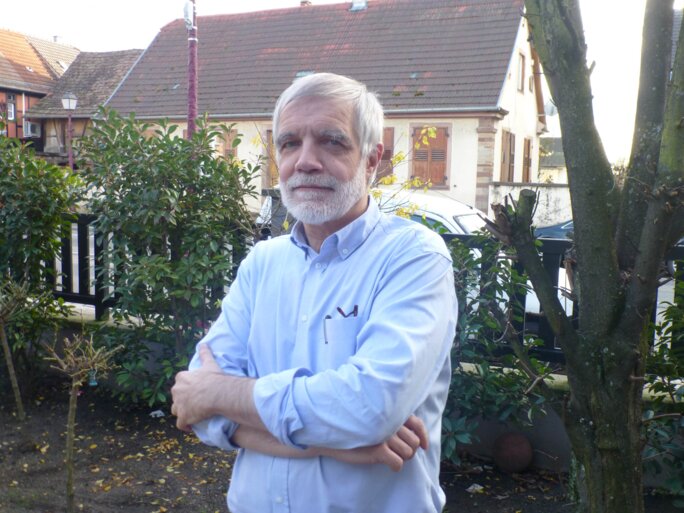
Enlargement : Illustration 3

This is not the first time that doctors who dissent from dubious hospital practices have had their reputations tarnished. Back in 1978, Dr. Olivier Rouhansky was the first to blow the whistle on French drug company Laboratoires Servier, which has since been implicated in France's biggest drug scandal over the slimming drug Mediator, accusing it of misleading publicity. Dr. Rouhansky had published research on Pondéral, an amphetamine derivative sold by Servier as an appetite suppressant. “When I started at Strasbourg CHU [Rouhansky] was considered mad and no one would work with him,” recalls Professor Marescaux, who admits the story has made a “strong impression” on him.
The Strasbourg professor has received support from a prominent whistle-blower, Dr. Irène Frachon, the lung specialist whose 2010 book, 'Mediator 150 mg: How Many Dead?' sounded the alert over the drug, which Servier was then discreetly pulling off pharmacy shelves. Her support, she explains, is not based on the details of the case, which she does not know, but on her experience of numerous cases of doctors who “question the hospital institution and the medical profession [and] are intimidated, silenced, sidelined. Harassment techniques are employed very quickly. It is totally violent.”
Hospitals and the medical profession react as collective bodies, she says. “Individually, these are often good people. But they are defending themselves against the violence of this profession, which can have very serious legal consequences. When the Mediator scandal broke, most doctors were less worried about the patients than about the court cases. A lot of doctors believe that accidents are the price you pay – you cannot make an omelette without breaking eggs.”
The plight of whistleblowers is the subject of a new book by human rights lawyer William Bourdon, Petit manuel de désobéissance civile ('Handbook of civil disobedience'), in which he recounts “the venom and the mud” thrown at them to undermine their testimony. He describes, too, what whistleblowers and their families suffer as a result of these “campaigns to discredit them”, adding that they need to be “vigilant” and “evaluate by all possible means” the impact their revelations will have.
In April Bourdon co-wrote an opinion piece in Le Monde with Mediapart editor-in-chief Edwy Plenel and Gerard Ryle, director of the International Consortium of Investigative Journalists (ICIJ), calling for a global platform to protect whistleblowers. And he has agreed to defend Dr Tanquerel, in Saint-Malo. Bourdon says faced with the growing rigidity of hospital managements and the isolation of whistleblowers, an independent authority is needed to monitor this area of public life.
That idea had already been floated by the Assises du Médicament, a grouping of specialists set up in the wake of the Mediator scandal to consult widely over reinforcing public health and drug safety. It proposed “creating a [legal] status for whistleblowers”, giving a “compulsory time limit” for public health authorities to respond to allegations and the setting up of an appeals body. But these recommendations have not been put into practice. A law initiated by the French green alliance Europe Ecologie - Les Verts (EELV) to create a national ethics commission for whistleblowing on health and environmental issues, the Commission nationale de la déontologie et des alertes en matière de santé et d'environnement, was passed on April 16th, 2013. But the decree implementing it was never issued so the body never came into being.
--------------------------------------------------------
- The French version of this article is here.
English version by Sue Landau
Editing by Michael Streeter


