A general practitioner has described how he used to spend hours in front of his computer at home, conducting back-to-back remote medical consultations with patients at a frantic pace. “I was doing as many as nine or ten consultations per hour; it was quite unbelievable,” recalls the family doctor, who nevertheless insists that he never rushed his work. “In 95% of telephone consultations, the conditions treated can be managed with ten standard prescriptions,” explains the GP, who has become highly critical of this model of healthcare provision.
This doctor wishes to remain anonymous, as the healthcare provider he used to work for, Livi, carries considerable clout: the Swedish company is one of the largest players in remote healthcare consultations across Europe. And several major global financial institutions are among its backers: the Ontario Teachers’ Pension Plan (OTPP), Index Ventures, Accel, Creandum, and Project A, who are pension and investment funds from Canada, the United States, Sweden and Germany.

Enlargement : Illustration 1

Indeed, the main remote healthcare providers are all backed by financial players of this kind. Qare, which claims to be the leader in so-called teleconsultation in France, was created in 2017 with the support of Kamet Ventures, the financial arm of giant insurance firm Axa. Medadom, another prominent name in remote healthcare providers in France, is backed by G Square Capital, a London-based investment fund.
In 2023, Ramsay, the largest group of private clinics in France, and which is itself owned by investment funds, also sought to get into this growing market. The group announced the creation of a subscription at 11.99 euros a month for “access to a doctor 7 days a week, 24 hours a day”. The announcement caused an immediate outcry, with unions representing France's many private or self-employed doctors dubbing it the “Netflix of healthcare”. Ramsay ultimately shelved the idea.
“This is fast-food medicine. It's turned general practice consultations into just another consumer good,” laments the doctor who worked for Livi for two years. He points to the fact that, as he himself only discovered towards the end of his contract, patients had the option to rate his work.
In response to Mediapart's questions, Livi acknowledged the highly demanding pace of its doctors' work, noting that its remote consultations on average last “ten minutes and thirty seconds”, compared to sixteen minutes face to face in a GP's surgery. However, the company explained that this shorter duration is made possible by “pre-consultation questionnaires” and by a “smaller administrative burden”.
According to Livi, its model helps combat social and regional healthcare inequalities. “Some 39 % of Livi patients live in a medical desert [editor's note, the expression used to describe regions where there is a shortage or lack of family doctors], and 26% of patients treated are covered by additional healthcare solidarity cover [editor's note, a public health insurance scheme for people on low incomes], compared with 10% in the general population,” it said. Livi also insisted that its doctors are the “same as those working in private practices, health centres or hospitals”.
6.24 minutes per consultation
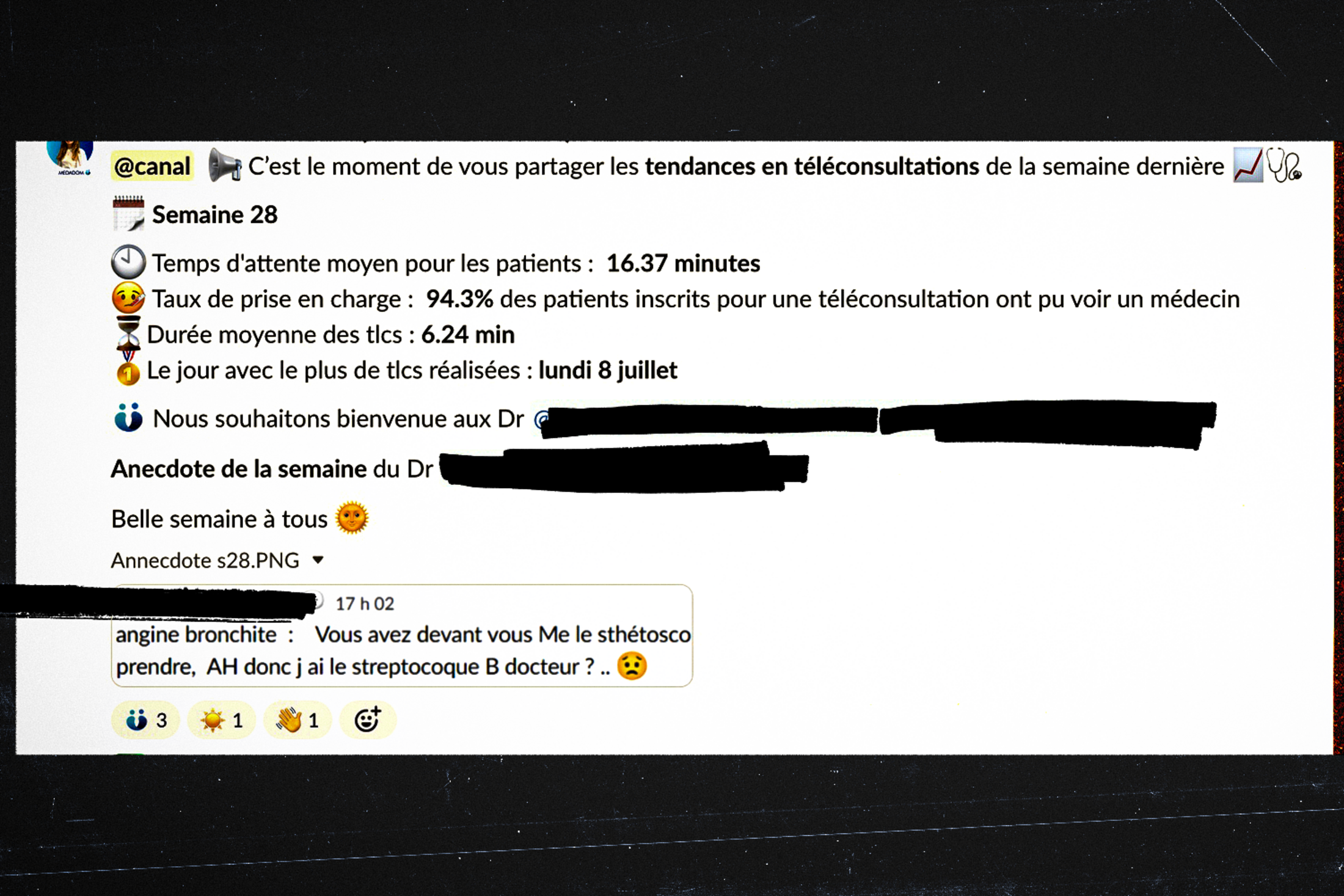
Yet, these doctors work under entirely different conditions - as part-time employees. And at Medadom at least, another major player in the sector in France, there are strong incentives to boost productivity. Employment contracts at Medadom, several examples of which Mediapart has obtained, set pay levels that correspond to four to five consultations per hour under normal private practice conditions. But these contracts also include adjustable pay if the doctor's revenue exceeds a specific target.
According to Mediapart's information, doctors at Medadom are also overseen by “medical business managers” who regularly review their activity – specifically, the “business” side of things. On top of this they frequently receive messages providing updates on overall activity. For instance, in one of these communications, which Mediapart has seen, the average duration of teleconsultations (“tlcs”) during week 28 was reported as 6.24 minutes.
Enlargement : Illustration 2
“During the Covid period, the public authorities opened the floodgates,” says an angry Christophe Lamarre, a general practitioner in Roubaix in northern France. Indeed, in March 2020, the state health insurance system opted to reimburse patients for 100% of the money they paid out on teleconsultation services. It was only in October 2022 that this reimbursement rate was reduced to 70%, aligning it with standard in-person consultations (in France people typically take out additional private health insurance to cover the remaining 30% or so of their healthcare bills that is not covered by the state health insurance system).
“Companies offering 24/7 access to a doctor, in my opinion that's unjustifiable. If someone needs a doctor at 3am but isn’t unwell enough to go to the accident and emergency department then it’s something that can wait until the morning. It’s a bit like an ‘Amazon doctor’,” he argues.
Livi, whose services are available “7 days a week from 6 am until midnight”, takes the opposite stance, asserting that this model “enables patients far from healthcare facilities to consult a doctor quickly outside of working hours or [avoids the need for them] to visit A&E”.
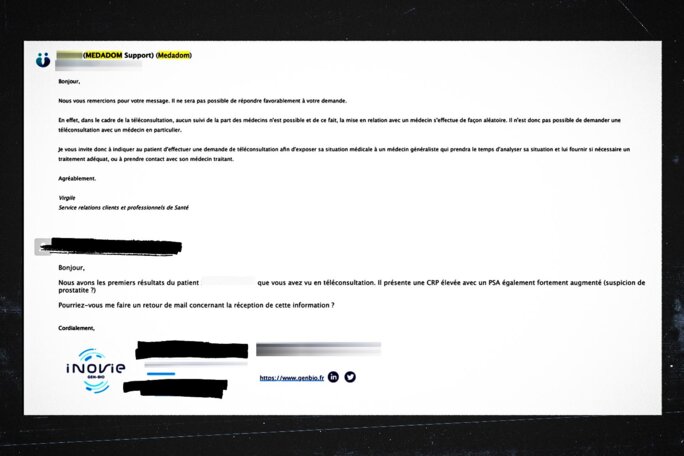
With teleconsultation, no follow-up with doctors is possible, hence patients are connected to a doctor randomly.
In the opinion of Amaury, a clinical pathologist from Saint-Étienne in south-east France, these providers falsely position themselves as an alternative to accident and emergency departments. “I’ve encountered cases where I had questions about tests prescribed during teleconsultations. I tried to contact the provider to speak with the prescribing doctor, and the only response I received was outright refusal. In the end, I had to send those patients to accident and emergency for a simple medical opinion.”
In an email exchange that Mediapart has seen, the service provider in question - Medadom, one of the three leaders in the French market - confirmed that “with teleconsultation, no follow-up with doctors is possible, hence patients are connected to a doctor randomly”.
Enlargement : Illustration 3
In its annual “income and outgoings” report for 2025, Assurance Maladie, the state health insurance organisation, dedicated an entire chapter to the use of remote consultations. Its data confirms accounts given by doctors. While between 2020 and 2023 - the latest available period for data - the overall number of teleconsultations declined from 17 million to 11 million, this drop relates to teleconsultations carried out by doctors working in their normal individual practices. In reality, independent providers are taking over the market: in 2023, they accounted for more than half of teleconsultations. In all, some 52% of remote consultations conducted by GPs took place via these providers. Among specialists, this figure was more than 80%.
Antibiotic prescriptions far more frequent
The report also highlights an issue that has been troubling the medical community for several years. Antibiotic prescriptions following a remote consultation are significantly more common when the consultation takes place via a specialist provider compared to when a doctor remotely consults a patient they already know.
For instance, according to the state health insurance system's data, among patients aged 70 to 74, around 8% of remote consultations by a doctor not using an independent provider result in an antibiotic prescription. In contrast, this figure soars to 20% for the same age group when the consultation occurs via a specialist provider. Assurance Maladie notes that the overprescription of antibiotics is “responsible for an increase in bacterial resistance”.
The doctor who previously worked with Livi admits to having been somewhat more liberal with antibiotics during remote consultations, as well as with other treatments and tests. “When you’re teleconsulting, you practise a defensive kind of medicine, prescribing more to protect yourself legally,” he explains. “I always told myself that in these cases, if something is missed, the only person who’s going to scrutinise my prescription is the judge,” he adds.
“There's also an issue with on-call healthcare hours,” Assurance Maladie told Mediapart. Evening, night-time and weekend slots, which are better reimbursed by the state health insurance, are highly lucrative for the specialist providers. “When I was at Livi, all the doctors rushed to grab the evening and night shifts because consultations during those hours were billed at 60 euros,” says the former Livi employee. In his view, the “entire financial model of these platforms relies on those higher-paid slots”.
Indeed, according to the state health insurance system’s “income and outgoings” report, 20% of remote consultations carried out by specialist providers take place in the evenings and at weekends, with no regulation. The state health insurance authorities appears determined to “tighten controls over these practices”. Assurance Maladie informed Mediapart that, starting from January 1st 2025, evening and weekend teleconsultations will no longer be paid at 60 euros but at a reduced rate of 35 euros. This lucrative income stream will therefore dry up.
In the meantime, Dr Lamarre in Roubaix says he is being “harassed” by emails from providers offering him “5,000 euros just for signing a contract”.
--------------------------------------------------------------------------------
- The original French version of this article can be found here.
English version by Michael Streeter


